The thing is, it’s not possible to cheat in diabetes. The word doesn’t make sense.
We can cheat ourselves, but that’s about it. The rest are just choices.
There’s no way to bully or make our way to the top in diabetes. It’s only about how we feel, how productive we are, and how much living we do.
The numbers don’t prove anything else. They don’t represent our worth or value (I think that’s the same thing). They are not a reflection of how good or successful a person we are.
Cheating may apply in games, class, sports, at work, with the IRS, or other places in life, just not in diabetes.
If we talk about cheating in diabetes, we are sending the wrong message. Let’s turn it around and talk about informed choices and engagement in care decisions/actions. This is true for those living with diabetes and talking about themselves, as well as for family, friends, strangers, and those in health care professions.


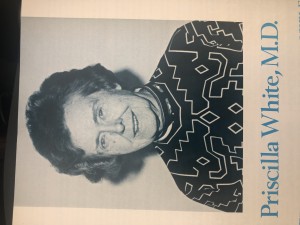
 In 1975, Priscilla White received the ADA’s award for Outstanding Service to Diabetic (sic) Youth. Maybe they didn’t have an award for service to mothers with diabetes. Dr. White started at the Joslin Diabetes Center in 1925 – only four years after insulin was isolated in Canada – and she worked tirelessly to improve infant survival rates for mothers with diabetes. Here’s a snapshot of her work:
In 1975, Priscilla White received the ADA’s award for Outstanding Service to Diabetic (sic) Youth. Maybe they didn’t have an award for service to mothers with diabetes. Dr. White started at the Joslin Diabetes Center in 1925 – only four years after insulin was isolated in Canada – and she worked tirelessly to improve infant survival rates for mothers with diabetes. Here’s a snapshot of her work: